
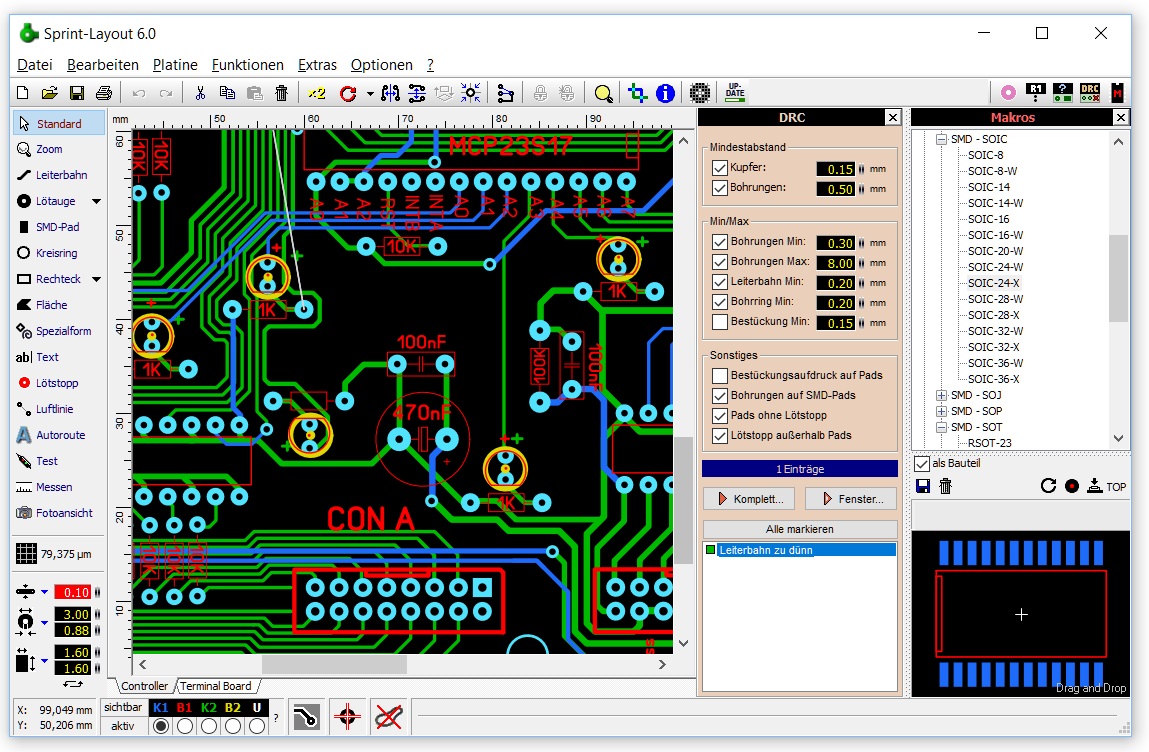
#Sprint layout 6.0 professional#
Planned follow-up is 3-6 years.īP measurements (sitting and standing), pulse, and BP-related information were collected using a standard automated BP device (the OMRON HEM-907 XL Professional Digital Blood Pressure Monitor). All clinics obtained institutional review board approval and each participant provided written informed consent. and Puerto Rico between Novemand March 15, 2013. Participants were recruited from 102 clinical sites across the U.S.
Individuals with diabetes, proteinuria ≥1 g/day, history of stroke, eGFR <20 ml/min/1.73m 2, symptomatic heart failure (HF) (within past 6 months), or left ventricular ejection fraction <35% were excluded. Patients with Framingham Risk Score >15, age ≥75 years, and/or CKD who met the BP eligibility criteria were automatically eligible for enrollment. Subclinical CVD criteria for enrollment within the past 2 years included left ventricular hypertrophy (LVH) ≥50% stenosis of a coronary, carotid or lower extremity artery abdominal aortic aneurysm (AAA) >5 cm with or without repair ankle brachial index (ABI) ≤0.90 and/or coronary artery calcium score ≥400 Agatston units. High risk was defined by clinical CVD (>3 month history) which included: MI, ACS, coronary revascularization, carotid endarterectomy/stenting, and/or peripheral artery disease (PAD) with revascularization. The protocol was designed to enroll three high risk subgroups: participants with CKD (eGFR 20-59 ml/min/1.73m 2) (target enrollment of 4,300), those with clinical or subclinical CVD (3,700), and seniors who were at least 75 years of age (goal of 3,250). The SPRINT recruitment target was 9,250, including additional targets of enrolling 50% women and 40% minorities. Participants are men and women aged ≥50 years with SBP between 130-180 mm Hg on 0-4 antihypertensive medications with at least one additional CVD risk factor. Secondary outcomes include all-cause mortality, ≥50% decline in kidney function (from baseline estimated glomerular filtration rate ) or development of end-stage renal disease (ESRD) among participants with baseline eGFR 20-59 mL/min/1.73 m 2, dementia, decline in cognitive function, and small vessel cerebral ischemic disease on magnetic resonance imaging (MRI). The primary endpoint is incident CVD events defined by the first on-study occurrence of a myocardial infarction (MI), acute coronary syndrome (ACS), stroke, heart failure (HF), or CVD death. Analysis by race (African Americans vs non-African Americans) is pre-specified in the protocol. In addition, the SPRINT Memory and cognition IN Decreased hypertension (SPRINT MIND) sub-study will test whether the lower SBP goal influences the rate of incident dementia and mild cognitive impairment, global and domain-specific cognitive function, and cerebral small vessel ischemic disease.
#Sprint layout 6.0 trial#
SPRINT is a two-armed, multicenter, randomized, open label, clinical trial designed to test whether a strategy to treat SBP to <120 mmHg will reduce cardiovascular disease (CVD) outcomes among non-diabetic hypertensive participants compared to treating to the currently recommended SBP target of <140 mmHg. The design and rationale of SPRINT have been reported previously and are summarized briefly. adults with hypertension were not controlled to the currently recommended target of 140/90 mmHg) at study entry among African Americans and non-African Americans. Despite antihypertensive treatment, nearly 50% of U.S.
The 2011-2012 National Health and Examination Survey (NHANES III) data suggested that 76% of US adults with hypertension were taking antihypertensives, with a higher percentage of African Americans (79.7%) than European Americans (76.6%). Despite recommendations on prescription of antihypertensive therapies, achieving BP control remains problematic and data on optimal BP targets remain controversial. Substantial data are available on the treatment and management of hypertension, with marked improvement in recent years in BP control rates, including incorporation in several guidelines.


 0 kommentar(er)
0 kommentar(er)
